Top 10 Most Asked Questions About the Liver — Expert Answers You Can Trust
The liver – your body’s remarkable chemical processing plant – performs over 500 vital functions that keep you alive and healthy. As one of your largest organs, it deserves our attention and care, yet many people remain confused about how it works and what can go wrong.
In this comprehensive guide, we’ll address the most common questions about liver health with evidence-based answers you can trust. Whether you’re concerned about hepatitis, curious about alcohol’s effects, or simply want to maintain optimal liver function, you’ll find clear, actionable information from medical experts.
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for personalized medical guidance or if you have concerns about your liver health.
1) What does the liver do?
The liver is truly your body’s metabolic powerhouse, performing hundreds of essential functions that keep you alive and healthy. This reddish-brown organ, weighing about 3 pounds in adults, sits just under your right ribcage.
Key liver functions include:
- Metabolism and energy production: The liver processes carbohydrates, converting them to glucose for immediate energy needs or storing them as glycogen for later use.
- Nutrient processing: Your liver metabolizes fats, proteins, and carbohydrates from digested food, transforming them into forms your body can use.
- Detoxification: The liver filters your entire blood supply approximately once per minute, removing toxins, medications, alcohol, and harmful substances.
- Bile production: The liver produces about a quart of bile daily to help digest fats and absorb fat-soluble vitamins (A, D, E, and K).
- Protein synthesis: Your liver manufactures essential blood proteins, including those responsible for blood clotting, immune system function, and maintaining fluid balance.
- Storage facility: The liver stores vitamins (A, D, E, K, and B12) and minerals (iron and copper) for when your body needs them.
This metabolic versatility makes the liver indispensable – there is no artificial device that can fully replace all liver functions.
2) What are the most common liver diseases?
Liver diseases affect millions worldwide, with varying causes, symptoms, and treatment approaches.
Viral Hepatitis
Hepatitis A: Caused by the hepatitis A virus (HAV), this infection spreads through contaminated food or water. While it causes acute inflammation, hepatitis A doesn’t lead to chronic liver disease and usually resolves without treatment.
Hepatitis B: This more serious infection spreads through blood, semen, and other body fluids. The World Health Organization estimates that 296 million people were living with chronic hepatitis B infection in 2019. Antiviral medications can control the virus, and vaccination is highly effective.
Hepatitis C: Hepatitis C virus (HCV) primarily spreads through blood contact. Modern direct-acting antiviral treatments can cure over 95% of cases, but many people remain undiagnosed until liver damage has occurred.
Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD):
This condition involves fat accumulation in liver cells without significant alcohol consumption. It affects an estimated 25-30% of adults in Western countries. Its more severe form, non-alcoholic steatohepatitis (NASH), involves inflammation and can progress to cirrhosis.
Alcoholic fatty liver disease:
Excessive alcohol consumption leads to fat accumulation, inflammation, and potentially alcoholic hepatitis and cirrhosis.
Other Common Liver Conditions
- Cirrhosis: The end stage of chronic liver damage, where healthy liver tissue is replaced by scar tissue, impairing function.
- Autoimmune hepatitis: The immune system attacks liver cells, causing inflammation and damage.
- Primary biliary cholangitis: A chronic disease that destroys the bile ducts in the liver.
- Hemochromatosis: A genetic disorder causing excessive iron absorption and storage.
3) What symptoms suggest a liver problem?
Liver disease often develops silently, earning it the nickname “the silent killer.” Early detection through symptom recognition can make a crucial difference in treatment outcomes.
Early Warning Signs
- Fatigue and weakness: Persistent tiredness that doesn’t improve with rest.
- Digestive discomfort: Nausea, reduced appetite, and abdominal discomfort, particularly in the upper right quadrant.
- Unexplained weight loss: When the liver can’t process nutrients properly.
- Cognitive changes: Mild confusion, trouble concentrating, or changes in sleep patterns.
More Advanced Symptoms
- Jaundice: Yellowing of the skin and eyes due to bilirubin buildup is a hallmark sign of liver dysfunction.
- Dark urine and pale stools: Changes in elimination can signal bile flow problems.
- Bruising and bleeding easily: The liver produces clotting factors, so impaired function can lead to unusual bruising.
- Fluid accumulation (ascites): Swelling in the abdomen or legs occurs when the liver can’t produce enough albumin protein.
- Itchy skin: Bile salt buildup under the skin can cause persistent itching without a rash.
Research from the British Liver Trust suggests that up to 75% of people with liver disease may be undiagnosed, underscoring the importance of regular check-ups.
4) How is liver disease diagnosed?
Diagnosing liver disease requires a comprehensive approach combining clinical evaluation, laboratory tests, imaging studies, and sometimes tissue analysis.
Medical History and Physical Examination
Physicians look for risk factors such as alcohol consumption, medication use, family history, and exposure to hepatitis viruses, as well as physical signs including jaundice or enlarged liver.
Laboratory Testing
Liver function tests (LFTs) measure various enzymes and proteins:
- Alanine aminotransferase (ALT) and aspartate aminotransferase (AST): Elevated when liver cells are damaged
- Alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT): Elevated in conditions affecting bile flow
- Bilirubin: A byproduct that can cause jaundice when elevated
- Albumin: Decreases with chronic liver disease
- Prothrombin time (PT): Measures blood clotting ability
Additional blood tests may include tests for viral hepatitis, autoimmune markers, genetic conditions, and cancer screening.
Imaging Studies
- Ultrasound: Often the first imaging test for detecting fatty liver, tumors, and bile duct abnormalities
- FibroScan (transient elastography): Measures liver stiffness to assess fibrosis
- CT and MRI: Provide detailed visualization of liver structure and function
Liver Biopsy
Despite advances in non-invasive diagnostics, liver biopsy remains the gold standard for definitively diagnosing many liver conditions by examining tissue under a microscope.
5) What are liver function tests (LFTs)?
Liver function tests are a panel of blood tests that provide valuable information about liver health and function.
Key Components of Liver Function Tests
Enzymes that indicate liver cell damage:
- ALT and AST: Elevated levels suggest liver cell injury
Enzymes related to bile duct function:
- ALP and GGT: Elevated levels may indicate bile duct obstruction
Markers of liver’s synthetic function:
- Albumin: Low levels may indicate chronic liver damage
- Prothrombin time (PT): Prolonged values suggest decreased liver synthetic function
Bilirubin metabolism:
- Total and direct bilirubin: Elevated levels cause jaundice
Interpreting Liver Function Tests
Different patterns suggest different conditions:
- Hepatocellular pattern: Predominantly elevated aminotransferases suggest liver cell damage
- Cholestatic pattern: Primarily elevated ALP and GGT indicate problems with bile flow
- Mixed pattern: When both types of markers are elevated
It’s important to note that normal LFTs don’t completely rule out liver disease, as early-stage conditions can present with normal or minimally elevated enzymes.
6) Can the liver regenerate itself?
The liver possesses a remarkable capacity for regeneration that distinguishes it from most other organs in the human body.
The Science Behind Liver Regeneration
After damage or partial removal:
- Cellular proliferation: Remaining healthy hepatocytes divide rapidly
- Growth factor activation: Molecules coordinate the regenerative response
- Vascular reorganization: Blood vessel networks reform
Studies show that after surgical removal of up to 70% of a healthy liver, the organ can regrow to near-normal size within 8-15 days.
Limitations of Liver Regeneration
While impressive, liver regeneration has important constraints:
- Quality over quantity: The regenerated tissue may lack the precise organization of the original liver
- Chronic damage effects: With ongoing injury, regeneration becomes impaired as scar tissue forms
- Advanced cirrhosis: Once cirrhosis becomes advanced, regenerative capacity diminishes significantly
- Age factors: Regenerative capacity declines with age
Clinical Applications
The liver’s regenerative ability enables:
- Liver resection surgery: Removing portions containing tumors
- Living donor transplantation: Donating a portion of liver to someone with liver failure
- Regenerative medicine research: Developing new treatment approaches
7) What causes fatty liver disease?
Fatty liver disease, characterized by excess fat accumulation in liver cells, has become the most common chronic liver condition worldwide.
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is strongly associated with:
Insulin resistance and metabolic syndrome:
- Obesity: 51% of obese individuals have NAFLD
- Type 2 diabetes: 55-70% of patients develop NAFLD
- Dyslipidemia: High triglycerides and low HDL cholesterol
- Hypertension: Often co-exists with other metabolic risk factors
Genetic factors:
- The PNPLA3 gene variant increases risk by 3-4 fold
- Approximately 27% of NAFLD risk is attributable to heritable factors
Dietary patterns:
- High fructose consumption
- Excessive refined carbohydrates
- High saturated fat intake
Microbiome disruption:
- Alterations in gut bacteria composition can increase intestinal permeability
Alcoholic Fatty Liver Disease (AFLD)
Alcohol directly damages the liver through:
Toxic metabolites: Acetaldehyde damages liver cells and promotes fat accumulation
Altered metabolism:
- Increases fatty acid synthesis
- Decreases fatty acid breakdown
- Impairs fat export from the liver
Dose-response relationship:
- For men: Risk rises above 3 standard drinks daily
- For women: Risk increases above 2 standard drinks daily
Other Contributors to Fatty Liver
- Medications: Corticosteroids, amiodarone, methotrexate, and others
- Rapid weight loss: Can temporarily increase liver fat
- Nutritional deficiencies: Protein malnutrition, choline deficiency
8) When should someone see a doctor about liver health?
Symptoms Requiring Immediate Medical Attention
- Jaundice: Yellowing of skin or eyes
- Severe abdominal pain: Especially in the upper right quadrant
- Mental confusion or drowsiness: Possible signs of hepatic encephalopathy
- Swollen abdomen with fluid: Indicates advanced liver disease
- Vomiting blood: May indicate esophageal varices from portal hypertension
Risk Factors Warranting Screening
Even without symptoms, certain risk factors justify evaluation:
- History of excessive alcohol consumption
- Metabolic risk factors: Obesity, type 2 diabetes, metabolic syndrome
- Viral hepatitis exposure risks: Injection drug use, certain blood transfusions, etc.
- Family history of liver diseases
Abnormal Test Results Requiring Follow-Up
- Elevated liver enzymes: Even mild elevations warrant investigation
- Abnormal imaging: Incidental findings on ultrasound, CT, or MRI
Dr. Paul Martin, Chief of Hepatology at the University of Miami Miller School of Medicine, advises: “Early intervention for liver disease can be life-changing. Many conditions that would progress to cirrhosis or liver cancer can be halted or even reversed if caught early enough.”
9) How can I keep my liver healthy?
Maintaining liver health is achievable through lifestyle choices that reduce risk factors and support optimal liver function.
Nutrition for Liver Health
- Mediterranean-style eating pattern: Reduces fatty liver incidence by 36%
- Beneficial components:
- Coffee: 2-3 cups daily is associated with reduced fibrosis risk
- Omega-3 fatty acids: Help reduce liver fat and inflammation
- Antioxidant-rich foods: Combat oxidative stress
- Foods to limit: Added sugars, highly processed foods, excessive salt
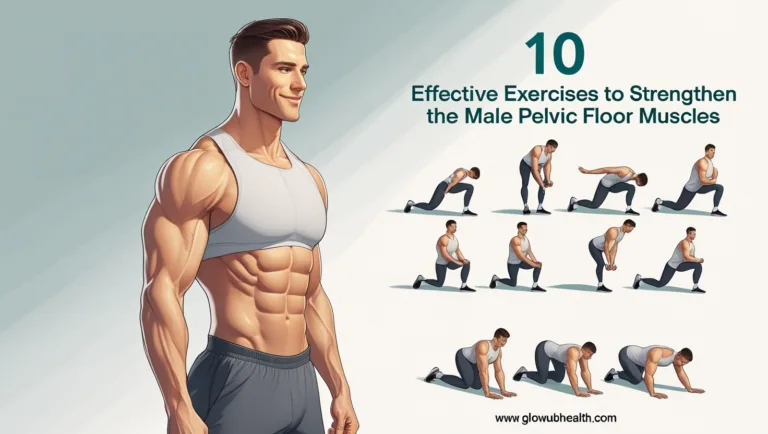
Physical Activity
Regular exercise:
- Reduces insulin resistance
- Decreases liver fat directly by about 30%
- Improves overall metabolic health
Recommendations include 150+ minutes of moderate activity weekly and muscle-strengthening activities at least twice weekly.
Weight Management
- Moderate, sustainable weight loss: Just 7-10% weight reduction resolves NASH in 90% of patients
- Avoiding rapid weight fluctuations: “Yo-yo dieting” can stress the liver
Alcohol Considerations
- Safe limits:
- Women: No more than 1 standard drink daily
- Men: No more than 2 standard drinks daily
- Regular alcohol-free days each week
Vaccination and Infection Prevention
- Hepatitis A and B vaccines: Safe and effective prevention
- Safe behaviors: Protection during sexual activity, avoiding shared needles
Medication Awareness
- Following prescribed dosages: Especially for acetaminophen
- Informing healthcare providers about all medications and supplements
- Avoiding unnecessary supplements: Some may cause harm
10) How does alcohol affect the liver?
The Liver’s Processing of Alcohol
- The liver uses enzymes to convert alcohol first to acetaldehyde (toxic) and then to acetate
- It can only metabolize approximately one standard drink per hour
Spectrum of Alcohol-Related Liver Damage
1. Alcoholic Fatty Liver (Steatosis):
- Fat accumulates in liver cells
- Completely reversible with abstinence
- Develops in over 90% of heavy drinkers
2. Alcoholic Hepatitis:
- Inflammatory condition with liver cell death
- Symptoms range from mild to life-threatening
- Mortality rates for severe cases reach 30-50% within 30 days
3. Alcoholic Cirrhosis:
- Advanced scarring that disrupts liver function
- Largely irreversible
- Develops in 10-20% of long-term heavy drinkers
Risk Factors for Alcohol-Induced Liver Disease
- Quantity and pattern: Daily drinking and binge drinking carry higher risk
- Gender differences: Women develop liver disease with less alcohol
- Genetic factors: Variations in metabolism genes
- Concurrent conditions: Obesity, viral hepatitis, diabetes increase risk
- Nutritional status: Malnutrition impairs liver regeneration
A landmark study in The Lancet found that there is no completely “safe” level of alcohol consumption for liver health, though risks remain very low with light, occasional drinking.
Conclusion: Prioritizing Your Liver Health
Your liver is truly a remarkable organ – silently performing hundreds of vital functions while asking for little attention in return. By understanding these top 10 questions about liver health, you’re now equipped with the knowledge to protect this essential organ throughout your life.
Remember that many liver conditions develop silently, making prevention and early detection crucial. The good news is that the most effective liver protection strategies are within your control: maintaining a healthy weight, eating a balanced diet, exercising regularly, limiting alcohol consumption, and getting vaccinated against hepatitis.
If you have risk factors for liver disease or experience concerning symptoms, don’t hesitate to speak with your healthcare provider. With prompt attention and lifestyle modifications, many liver conditions can be successfully managed or even reversed before permanent damage occurs.
Your liver works tirelessly for you every day – taking these steps to care for it is one of the most important investments you can make in your long-term health and wellbeing.
FAQ
1. What are signs of problems with your liver?
Common signs of liver problems include fatigue, jaundice (yellowing of the skin or eyes), dark urine, pale stool, abdominal pain or swelling (especially in the upper right side), nausea, and unexplained weight loss. If you notice any of these symptoms, it’s important to consult a healthcare professional.
2. What are 5 liver functions?
The liver performs many essential tasks. Five key functions include:
Detoxification of harmful substances from the blood.
Production of bile to aid in digestion of fats.
Metabolism of carbohydrates, proteins, and fats.
Storage of vitamins, minerals, and glycogen (a form of glucose).
Synthesis of blood proteins, such as albumin and clotting factors.
3. Do I have 1 or 2 livers?
Humans have one liver, but it is divided into two main lobes: the right and left lobes. It is the largest solid organ in the body and plays a crucial role in overall health.
4. What are the four warning signs of a dying liver?
The four serious signs that may indicate liver failure or a dying liver include:
Jaundice
Confusion or cognitive impairment (hepatic encephalopathy)
Swelling in the abdomen or legs (ascites/edema)
Severe fatigue and weakness
These are medical emergencies and require immediate attention.
5. Can you recover from liver scarring?
Liver scarring, or fibrosis, can be reversible in its early stages if the underlying cause (such as alcohol use or hepatitis) is treated. However, once it progresses to cirrhosis, the scarring is generally permanent, though further damage can be slowed or stopped with proper care.
6. What are the 4 liver markers?
Liver function is typically monitored using four main blood test markers:
ALT (Alanine aminotransferase)
AST (Aspartate aminotransferase)
ALP (Alkaline phosphatase)
Bilirubin
These markers help assess inflammation, bile flow, and the liver’s ability to process waste.
7. What are the symptoms of liver infection?
Symptoms of a liver infection (such as hepatitis) may include:
Fever
Jaundice
Fatigue
Loss of appetite
Abdominal discomfort (especially in the upper right)
Nausea or vomiting
Prompt diagnosis and treatment are key to managing liver infections.
8. How long does it take to detox the liver?
The liver naturally detoxifies the body daily. However, recovery from liver stress or overload depends on the cause. For example:
-After alcohol cessation, liver function can begin improving in a few weeks.
-With healthy lifestyle changes, noticeable improvements may be seen in 1 to 3 months.
There is no set timeframe, and claims of “rapid liver detoxes” should be approached with caution.